American
![]() f
Manual
Medicine
f
Manual
Medicine
|
American
|
Home
Search
Pain referral
Trigger points
Cranial nerve
Spinal nerve
Historical
About us
Contact us
Site map
There are four (4) muscles in the Suboccipital Group. They are the Rectus Capitis Posterior Major, Rectus Capitis Posterior Minor, Oblique Capitis Inferior, and Oblique Capitis Superior.
Anatomical Attachments: Action: Extension, lateral flexion and rotation of the head.
Synergist: Extension – Semispinalis Capitis; Rotation – Splenius Capitis; Lateral flexion – Rectus Capitis Lateralis.
Antagonist: Extension – Longus Capitis, Rectus Capitis Anterior;
Rotation – Oblique Capitis Inferior, Rectus Capitis Posterior Major;
Lateral flexion – Oblique Capitis Superior, Rectus Capitis Lateralis.
Nerve Supply: Dorsal division of the suboccipital, 1st cervical nerve.
Vascular supply: Vertebral and Occipital Artery.
Anatomical Attachments: Action: Extends and laterally flexes the head.
Synergist: Extension – Semispinalis Capitis; Lateral Flexion – Rectus Capitis Lateralis.
Antagonist: Extension – Longus Capitis, Rectus Capitis Anterior; Lateral Flexion – Oblique Capitis Superior, Rectus Capitis Lateralis.
Nerve Supply: Dorsal division of the suboccipital 1st cervical nerve.
Vascular supply: Vertebral and Occipital Artery.
Anatomical Attachments: Action: Rotates C1 and cranium.
Synergist: Rotation – Splenius Capitis
Antagonist: Rotation – Oblique Capitis Inferior, Rectus Capitis Posterior Major
Nerve Supply: Posterior primary rami of C1 & C2.
Nerve Entrapment: According to Simons, Travell and Simons, occasionally, the Oblique Capitis Inferior can entrap the Greater Occipital nerve.
Vascular supply: Vertebral and Occipital Artery.
Anatomical Attachments: Action: Extends and laterally rotates the head.
Synergist: Extension – Semispinalis Capitis; Rotation – Splenius Capitis
Antagonist: Extension – Longus Capitis, Rectus Capitis Anterior; Rotation – Oblique Capitis Inferior, Rectus Capitis Posterior Major
Nerve Supply: Dorsal division of the suboccipital 1st cervical nerve.
Vascular supply: Vertebral and Occipital Artery.
Vascular entrapment: According to Travell and Simons, the suboccipitals do not attribute to vascular entrapment. However, according to Philip Greenman D.O. the vertebral arteries traverses through the Transverse Foramen of the cervical vertebrae. After penetrating the foramen of C1 it traverses medially along the cranial surface of the posterior arch of C1, prior to it’s ascension through the foramen magnum and subsequent uniting with the other vertebral arteries to form the basilar artery and the circle of Willis. Therefore, it is not unreasonable to assume, that hypertonic suboccipital muscles can impinge blood supply as they pass over the posterior aspect of C1. If one of these arteries is occluded and the head is placed in extension and rotation, complete blood loss from the vertebral arteries may occur. This phenomenon can be self induced by looking over one’s shoulder when attempting to back up a car. Manipulative practitioners should never induce simultaneous cervical rotation and extension, as this has been attributed to causing Ischemic brain syndrome and vascular accidents.
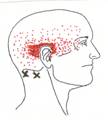
Click on a small image to view an enlarged image Trigger Point Signs and Symptoms: Severe headaches which can refer to the posterior eye, difficulty in rotating the head, neck pain, pressure to the occiput exacerbates symptoms.
Trigger Point Activating and Perpetuating Factors: As with all myofascial conditions sudden cooling, emotional stress, and mechanical overload exacerbate trigger points. With the suboccipitals, lateral neck bending such as cradling a phone under one’s ear, or persistent extension-hyperextension such as overhead painting, or viewing TV while lying on your stomach with your head propped up on your hands, are examples of poor ergonomics and perpetuating factors for TrPs.
Authors' note: There are several types of headaches. Usually headaches develop by an adverse stimulus, which poses no real threat to the individual. Migraine headaches have several forms basically there are two types; migraine headache without aura and migraine headache with aura. The migraine headache with aura is usually preceded with subjective motor or sensory phenomena, with visual disturbance being the most frequently referenced. Regardless whether the migraine headache is preceded with an aura or not, they generally are accompanied with at least three or more of the following: lacrimation, facial swelling, ptosis, hypersensitivity to light, sound or smell, and nausea or vomiting. They involve one half (1/2) of the cranium and may be persistent for 4 to 72 hours. They are frequently referenced as histamine or vascular headaches. According to several authors, cluster headaches may be a form of migraine headache. This is based upon the fact that only one half (1/2) of the cranium is involved. However, the duration is much shorter, with total duration ranging from 15 to 180 minutes. They derive their name due to the fact that while they last shorter in duration, their prevalence of onset appears to come in groups, with it not being uncommon to have as many as eight (8) a day. For some reason males seem to be more susceptible to cluster headaches, than the female population. Nevertheless, the pathophysiology of migraines and clusters are essentially the same.
Contemporary medical thought defines tension headaches as a mild to moderate headache which lasts from two (2) to eight (8) days and which predominantly affects the neck and occipital region. The predicating factor is either acute or chronic physical or emotional stress. However, based upon the works of Travell, Simons and others, as it pertains to perpetuating factors of trigger points and their referral patterns, it has been established that all regions of the neck, shoulder, and cranium may be affected by the activation of trigger points. Tension myalgia, a diagnosis initially rendered by the Mayo clinic to reference tension related low back and pelvic pain, has more recently been broadened to incorporate the neck, shoulder, and cranial pain as well. As hypertonic muscles can translate vertebrae, biomechanical nerve compression especially of C1 and C2 may also be attributed to the pathogenesis of tension related concomitants. There are numerous perpetuating factors for TrP activation. Obviously, persistent emotional and physical stress is the most frequently observed. However, TrPs may also be activated by the onset of trauma, toxicity, nutritional inadequacy, hormone imbalance and disease. Anytime an individual exhibits undiagnosed posterior eye or temporal pain, the practitioner should suspect a possible aneurysm, until diagnostically excluded. Below are listed several clinical considerations which may cause headaches or cranial pain.
Differential Diagnosis: Intracranial: Intracerebral Aneurysm, Cerebral hemorrhage, Thrombosis, Hypertension, Brain abscess, Encephalitis, Cerebral hematoma, Meningitis, Hydrocephalus, Transient Ischemic Attack (TIA or Ischemic Brain Syndrome), Cerebral Vascular Accident (Stroke), Rocky Mountain Spotted Fever, Vasculitis, Brain Tumor or Cancer, Optic neuritis, Concussion, Postconcussion syndrome, Temporal arteritis (Giant Cell Arteritis), Hypothyroidism, hangover, toxicity, Menses, Menopause. Extracranial: Cervical Osteoarthritis, C1 C2 or C3 Nerve compression, Occipitoatlantal articular dysfunction, Vertebral artery entrapment, Tension myalgia, Systemic Lupus Erythematosus, Paget’s disease, Visual Acuity change, Eye disease, Eye strain, Sinusitis, Allergic rhinitis, Common cold, influenza, Temporomandibular joint dysfunction, Toothache, Tetanus, Occipital neuralgia, Trigeminal neuralgia, Glossopharyngeal neuralgia, Otitis media, Mastoiditis, Acoustic Neuroma, Chronic fatigue syndrome, poor ergonomics, noisy or stuffy work environment, Anemia, Caffeine withdrawal, fever, Hypercapnia, Hypertension, Hypoxia, Herpes zoster (Ramsay Hunt’s Syndrome, Herpes zoster ophthalmicus, Herpes simplex keratitis), Heatstroke, Systemic infections or inflammation, Hunger (nutritional inadequacy), Certain foods or food additives, Change in the weather, fatigue, excessive sleep, Metabolic imbalance, Side effects of medication.
Home
Search
Pain referral
Trigger points
Cranial nerve
Spinal nerve
Historical
About us
Contact us
Site map
Continuing Education © Copyright
Suboccipital Muscle Group

Pointer Plus
Rectus Capitis Posterior Major

Rectus Capitis Posterior Minor

Oblique Capitis Inferior

Oblique Capitis Superior

The Suboccipital muscles as a Group
(Rectus Capitis Posterior Major, Rectus Capitis Posterior Minor, Oblique Capitis Inferior and Oblique Capitis Superior)
Travell and Simons Trigger Point Pain Referral:
The pain from the trigger points in the suboccipitals emanates from the most superior posterior aspect of the neck and occipital bone then traverses along the side of the head, to the posterior eye and forehead.